Glaucoma vs. Cataracts
Glaucoma and cataracts are two common chronic eye diseases—but they affect your eyes very differently. You can, however, have both cataracts and glaucoma. Cataracts may occur naturally with glaucoma, may affect your glaucoma, or may even occur as a result of having had glaucoma surgery. Learn about how these two chronic diseases affect your eye health.
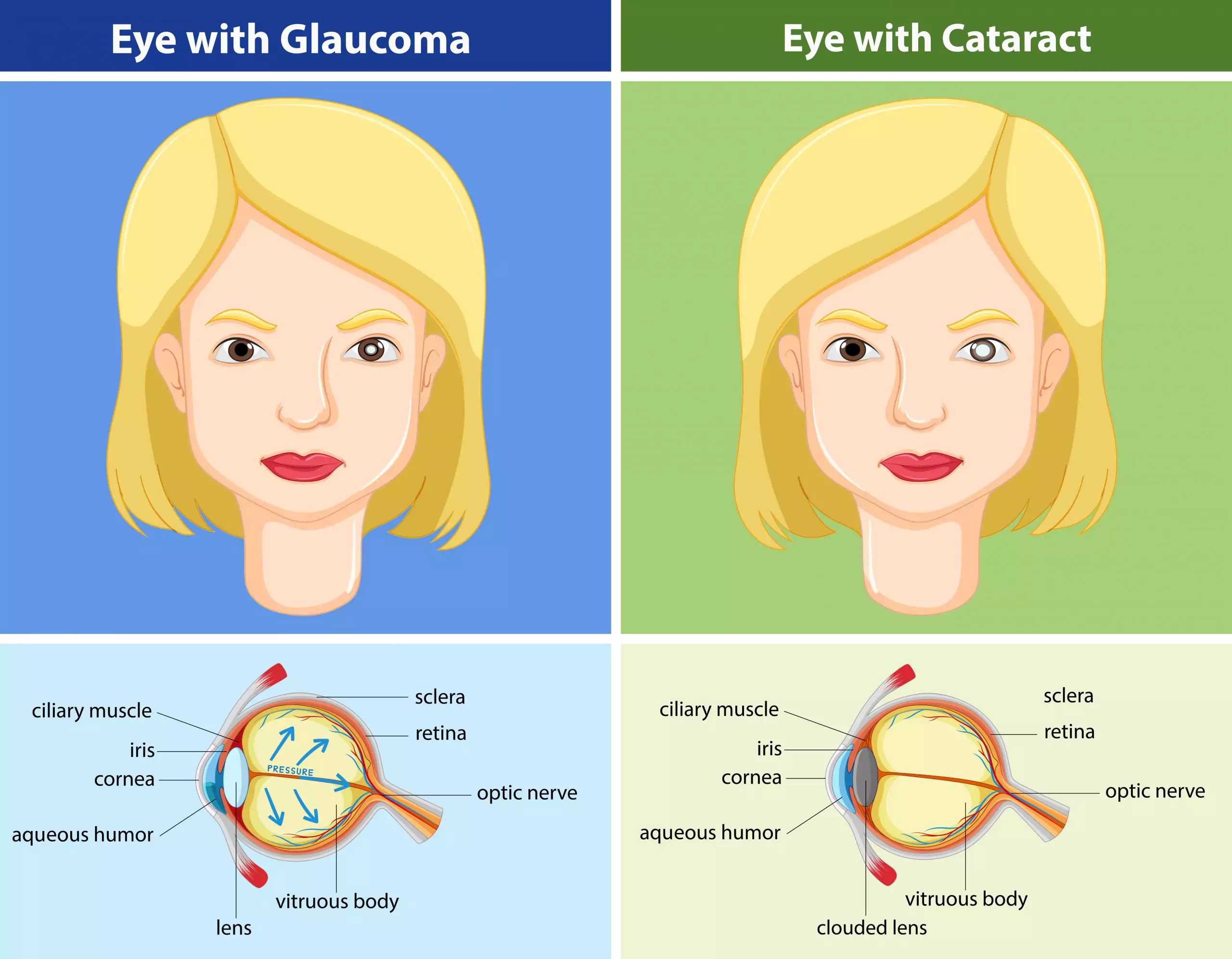
Comparison between glaucoma vs cataracts
Glaucoma
Glaucoma is a group of conditions that affects the optic nerve. When a fluid, called aqueous humor, builds up in the eye, it causes an increase in eye pressure, known as intraocular pressure (IOP). This occurs when there is either an overproduction of aqueous humor or your trabecular meshwork (the tissue through which this liquid drains) becomes blocked. High intraocular pressure (IOP) causes damage to the optic nerve, which, in turn, causes glaucoma. Typical symptoms of glaucoma include:
- Blind spots or patches in your peripheral (side) or central vision, often in both eyes
- Tunnel vision (in advanced stages)
- Eye pain
- Nausea and/or vomiting
- Severe headaches
- Blurred vision
- See halos around lights
- Redness of the eye
Even with treatment, both for symptoms and preventative care, glaucoma will progressively worsen over time. As stated by the Mayo Clinic, “If left untreated, glaucoma will eventually cause blindness. Even with treatment, about 15 percent of people with glaucoma become blind in at least one eye within 20 years.”
There are several diagnostic tests for glaucoma, including:
- Visual acuity test. Measures how clearly you see at various distances.
- Tonometry. Measures the pressure inside your eye.
- Pachymetry. Measures the thickness of your cornea.
Cataracts
Cataracts are very common, particularly as you get older, and are defined as a cloudy area in the lens of your eye. The lens is what allows light to enter your eye and project images to your retina at the back of your eye. When the proteins inside your eye break down, they can clump together to form the aforementioned cloudy area, typically white, yellow, or brown in color.
Many people with cataracts don’t notice them at first, but gradually, you will notice your vision getting blurry, hazy, and/or less colorful, as well as experience difficulty doing everyday activities, including reading.
Typical symptoms of cataracts include:
- Blurry or cloudy vision
- Poor night vision (night blindness)
- See colors as faded
- Feeling of lights being too bright (lamps, sun, headlights)
- See halos around lights
- See double (may go away as a cataract gets bigger)
- Frequent changes to your glasses prescription
While cataracts most often occur naturally, they can also happen after sustaining an injury to the eye or post-operation for a separate eye condition, such as glaucoma. The only way to treat cataracts is with surgery to get rid of them, but the surgery is safe and fully eliminates any cataracts-related vision issues. If left untreated, cataracts can lead to vision loss.
Summary of cataracts vs glaucoma
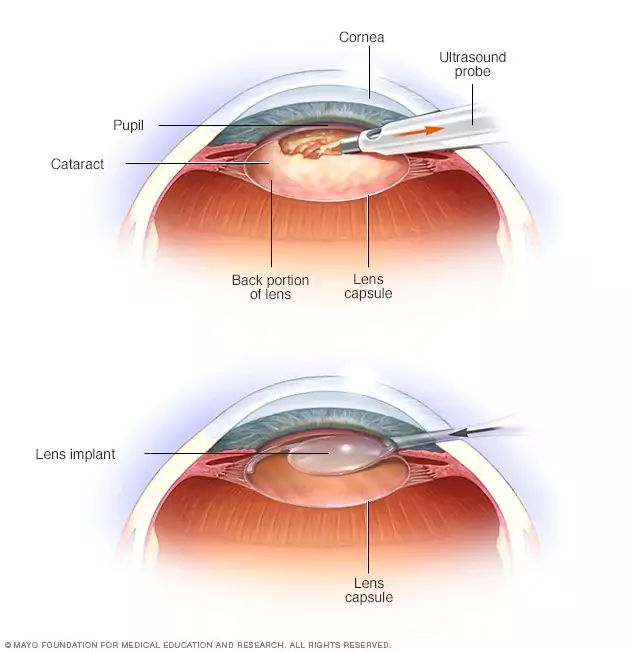
Here, you can see where and how cataract surgery is performed on the lens of your eye.
(This image is from the Mayo Clinic.)
- Glaucoma involves eye pressure and affects the optic nerve, whereas cataracts involve the breakdown of proteins and affect the lens.
- Cataracts are painless and happen over time, whereas glaucoma can be either slow and subtle or quick and painful, depending on the type of glaucoma and severity.
- Glaucoma can cause irreversible blindness, whereas vision loss is less likely with cataracts (albeit still possible).
- Vision loss in cataracts can be reversed with surgery, whereas it cannot with glaucoma surgery.
- Cataract surgery involves removing the lens and replacing it with an artificial lens, whereas glaucoma surgery uses a laser to open up the blocked canals that are preventing fluid drainage.
- Cataracts are not an urgent medical condition, whereas early prevention and treatment are crucial in glaucoma.
Are there any similarities between glaucoma and cataracts?
- Both glaucoma and cataracts can cause vision loss.
- Both of these eye diseases happen more commonly in people with diabetes.
- Surgery is a treatment option for both glaucoma and cataracts. (It’s important to note, however, that it’s not the first course of treatment in glaucoma. It is usually only performed when other treatment methods, such as eye drops, are insufficient.)
Do cataracts affect glaucoma and vice versa?
Cataracts can become so large in size that they block your eye’s drainage system, requiring a similar surgery to glaucoma. Cataracts can also form after glaucoma surgery. As Healthline reports, “researchers recommend that you wait 1 to 2 years after certain glaucoma surgeries to have surgery on a cataract. The delay can help ensure that your eye is healthy and stable before you have cataracts removed.”
Can glaucoma and cataract surgery be done together?
It is possible to have surgery for both cataracts and glaucoma at the same time. These operations include:
- Trabeculectomy
- Glaucoma drainage devices
- Canaloplasty
- Endocyclophotocoagulation
- Micro-invasive glaucoma surgeries (MIGS)
The most commonly performed combination surgeries are the newer MIGS procedures; this is because both the cataract and glaucoma surgery can typically be performed through the same incision. For certain patients, such as those with narrow-angle glaucoma, it’s possible that cataract surgery may improve drainage and alleviate high IOP and prevent a need for glaucoma surgery.
To determine whether a combined surgery is right for you, you must meet with your doctor and care team. There are a number of variables to consider, as well as other treatment options. Your doctor will take into consideration your unique case, including the type of glaucoma you have and the severity of it, to decide which, if any is the right surgical approach for you.
Do you have glaucoma or know someone with this chronic eye disease? Learn more on The Glaucoma Community

