How to Treat Low Kidney Function
Although there is no cure for chronic kidney disease (CKD), your doctor can work with you to treat and manage your existing symptoms, reduce underlying issues, and find ways to slow down disease progression. Some of the treatments are universal, while others depend upon the stage of CKD you are in.
A healthy diet and lifestyle combined with appropriate medications for symptom control is the most common treatment for kidney disease in its early stages. Renal replacement therapy, such as dialysis or a kidney transplant, is reserved for end-stage kidney disease (ESKD).
Nutrition and low kidney function
Food is what our bodies use for growth, homeostasis, and healing. This is why it’s important for you to consult with a dietician who is knowledgeable about kidney disease. You’ll need to find and maintain a balance between the levels of electrolytes, minerals, and fluid in your body.

A modified diet for chronic kidney disease may include adjustments to your intake of the following food items:
- Sodium: Sodium raises blood pressure, and high blood pressure (hypertension) is a primary cause and complication of CKD. Sodium is widely used as a preservative. Your intake can be reduced by eating fresh and minimally processed foods instead of canned or pre-packaged ones.
- Protein: When metabolized, protein creates wastes that the kidneys may no longer be able to process optimally. Reducing your protein intake can decrease the burden on your kidneys. If and when you start dialysis, however, you may need to increase your protein intake again.
- Alcohol: Alcohol can raise your blood pressure and cause dehydration—both of which are especially dangerous for people with CKD. As a liquid, alcohol must also be added to the equation when calculating your fluid intake.
- Minerals: When you have CKD, your kidneys can’t process certain minerals, such as phosphorus and potassium, efficiently. Too much phosphorus in your blood can leach calcium from your bones, leaving them weak and brittle. Dairy products are high in phosphorus, so your doctor may limit your dairy consumption.
- Calories: Dietary limitations, along with an often severe and prolonged loss of appetite, can lead to malnutrition. Thus, it’s important to consume enough healthy calories daily.
- Sugar: Sugar can help with your short-term energy, but it can also be dangerous if you have diabetes or are prediabetic. Like hypertension, diabetes is both a cause and a complication of chronic kidney disease. Your doctor may reduce your sugar intake.
- Dietary supplements: People with CKD often have insufficient amounts of vitamins and minerals in their blood. Your healthcare provider may prescribe oral or intravenous dietary supplements, such as vitamin B1, B2, B3 (niacin), B5 (pantothenic acid), B6, B9 (folic acid), B12, biotin, vitamin C, iron, and/or calcium. Do not attempt to supplement without consulting your physician. Different dosages can have positive or negative effects.
Stay on top of your CKD
Responsum for CKD empowers people with kidney disease through community, knowledge, and shared experiences
Medications and low kidney function
Medications make up the next layer of both offense and defense in the treatment of low kidney function. They are frequently used to control common symptoms and related medical conditions of chronic kidney disease.

These conditions and symptoms include:
- Anemia: Anemia may develop at any stage of CKD. Damaged kidneys don’t make enough of the hormone erythropoietin (EPO), so your bone marrow makes fewer red blood cells. This can cause weakness, fatigue, and a feeling of being constantly cold. You may be prescribed supplemental erythropoietin and/or iron supplements orally or intravenously to manage these symptoms.
- Cholesterol: People living with CKD frequently have high levels of “bad” cholesterol (LDLs, or low-density lipoproteins). High LDLs increase your risk of stroke and of developing heart disease—the leading cause of death for people with CKD. Medications, called statins, may be prescribed to help control your LDL levels. Exercise, if done safely, can also help reduce cholesterol and blood pressure. This can help prevent heart disease and slowing disease progression, particularly in stages 3 and 4.
- Edema: People with kidney disease often retain fluids. This results in swelling (edema), particularly in the hands, legs, and face. Fluid retention also increases blood pressure. Medications, called diuretics, can help you flush excess water from your system and regain fluid balance.
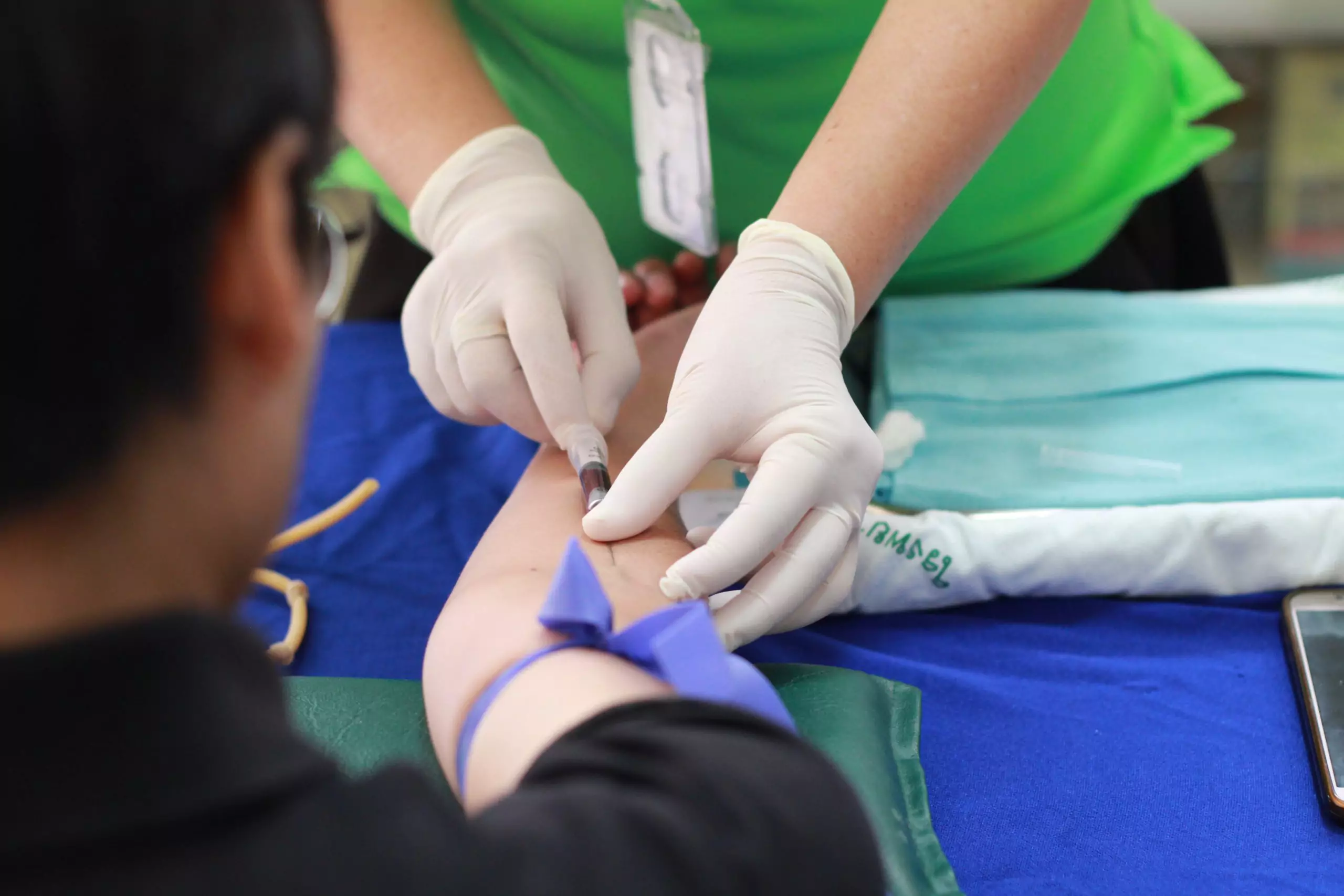
- High blood pressure: In addition to reducing your sodium and alcohol intake, your healthcare provider may prescribe medications to help lower your blood pressure. Common blood pressure medications include angiotensin-converting enzyme (ACE) inhibitors and angiotensin II receptor blockers (ARBs). These medications can initially lower kidney function and change electrolyte levels, so your doctor may monitor your response closely and order frequent blood tests.
- Weak and/or brittle bones: Excess phosphorous in the blood can cause calcium loss in your bones, and calcium buildup can cause your blood vessel to calcify. To counteract this, your healthcare provider may prescribe calcium and vitamin D supplements, as well as a phosphate-binding medication.
Procedures and low kidney function
Diet modification and medications can help delay the progression of chronic kidney disease, especially in the early stages. If the disease progresses, however, other forms of treatment may become necessary.
Other forms of treatment may include:
- Blood transfusions: Hormone and iron supplements are not always enough to manage the symptoms of anemia. In those cases, your doctor may order one or more blood transfusions.
- Dialysis: Dialysis is an artificial method of removing wastes, toxins, and excess fluids from your blood when your kidneys cease to function. There are two types of dialysis: hemodialysis and peritoneal dialysis.
- With hemodialysis, your blood is filtered through a machine to be cleansed of impurities and then returned to your body.
- With peritoneal dialysis, a thin tube (catheter) is inserted into your abdomen, which you fill with a solution that absorbs wastes and extra fluids. After a specified period of time, the solution is drained, and the wastes are removed.
- Kidney transplant: If a healthy donor kidney is available, it is surgically placed and attached inside your body. Daily medications are necessary to prevent your body’s rejection of the new kidney.
Experimental treatments for CKD
Research is ongoing to find new treatments and interventions that will someday soon render dialysis and kidney donation unnecessary. The Harvard Stem Cell Institute is just one of many institutions exploring a wide variety of options, such as experimental treatments.
Harvard’s current kidney disease research path has three tiers:
- Short-term: This research is intended to repair damaged kidneys by using regenerative medicine—or cell replacement therapy—using mesenchymal stem cells (cells found in bone marrow). These cells are our body’s natural defense against kidney damage.
- Medium-term: This involves identifying the types of kidney cells most susceptible to damage in order to target the specific cell types with appropriate medications.
- Long-term: The long-term goal is to use stem cells and nanotechnology to create an artificial kidney that can be used in transplant surgeries—eliminating the need to rely solely on human kidneys. Thus far, scientists have created a rat kidney that is being tested on lab animals.
Clinical trials are also being run by the National Institutes of Health (NIH) and the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) to test the effectiveness and safety of pirfenidone in the treatment of diabetic nephropathy.
Pirfenidone is an anti-scarring drug used to treat idiopathic pulmonary fibrosis. Scientists hypothesize that the drug may prevent or treat the scarring that occurs in diabetic people’s kidneys as a result of protein accumulation. In this way, it could stabilize and preserve kidney function in kidney disease patients with either type 1 or type 2 diabetes.


