Polycystic Kidney Disease: Symptoms, Diagnosis, and Treatment
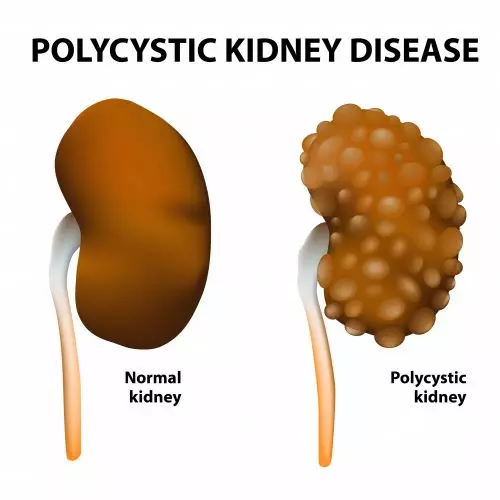
Polycystic kidney disease (PKD) is a rare genetic disorder that affects the kidneys, causing the formation of fluid-filled cysts that can lead to kidney damage and, in severe cases, kidney failure. About 500,000 people in the U.S. are affected by PKD, including children. Learn about the various aspects of PKD, including its causes, symptoms, diagnosis, treatment options, and the importance of early detection.
Understanding polycystic kidney disease
PKD is a hereditary condition characterized by the development of cysts in the kidneys. These cysts are noncancerous, fluid-filled sacs that can vary in size and number. PKD is typically divided into two main types: autosomal dominant (ADPKD) and autosomal recessive (ARPKD).
- Autosomal dominant PKD. ADPKD is the more common form of PKD, affecting approximately 90% of individuals with PKD. It’s an inherited condition caused by mutations in either the PKD1 or PKD2 gene. These mutations lead to the development of cysts in the kidneys, which can grow over time and affect kidney function.
- Autosomal recessive PKD. ARPKD is a rarer and more severe form of PKD that typically presents in infancy or early childhood. Unlike ADPKD, it is caused by mutations in the PKHD1 gene and can also affect other organs, such as the lungs and liver.
Causes and risk factors of PKD
If one or both of your parents have PKD, there is a chance that you may inherit the condition. The specific genes responsible for PKD (PKD1 and PKD2) are located on different chromosomes. Mutations in either of these genes can lead to the development of cysts in the kidneys.
Though PKD is primarily a genetic condition, there are several risk factors that can influence its development, severity, and progression:
- Age. PKD symptoms may not appear until adulthood, even in people born with the genetic mutation.
- Gender. PKD affects both males and females equally.
- Lifestyle factors. High blood pressure and smoking can exacerbate the progression of PKD, and should be addressed and managed early and carefully.
Symptoms of PKD
The symptoms of PKD can vary widely among affected individuals, and they often depend on the type of PKD, the size and number of cysts, and the overall health of the kidneys. Common symptoms include:
- Dull, aching pain in the abdomen, back, or sides
- Enlarged kidneys
- Frequent urinary tract infections (UTIs)
- Hematuria (blood in the urine)
- High blood pressure
- Kidney stones (from obstructed urine flow)
- Proteinuria (excessive protein in the urine, indicative of kidney damage)
Stay ahead of your CKD
Responsum for CKD empowers people with kidney disease through community, knowledge, and shared experiences
Diagnosing PKD
If you or a loved one experience symptoms that could be related to PKD, it is essential to seek medical evaluation. Diagnosing PKD typically involves a combination of the following:
- Medical history. Your healthcare provider will inquire about your personal health history, as well as your family members’ health history.
- Physical examination. A physical exam can help identify signs of kidney enlargement or tenderness.
- Imaging studies. Ultrasound, CT scans, or MRI scans are commonly used to get a clear picture of the kidneys and detect cysts.
- Genetic testing. Genetic testing can confirm the presence of PKD and identify the specific gene mutation responsible.
Treatment options for PKD
There is currently no cure for PKD, but various treatment options are available to manage its symptoms and slow the progression of the disease. Treatment strategies focus on:
- Blood pressure management, through medications like angiotensin-converting enzyme (ACE) inhibitors or angiotensin II receptor blockers (ARBs)
- Pain management, with over-the-counter pain relievers or prescription medications
- Lifestyle modifications, such as a low-salt diet, regular exercise, and avoidance of tobacco and excessive alcohol consumption
- Treating complications like kidney stones or urinary tract infections
In severe cases that lead to kidney failure, dialysis or kidney transplantation may be necessary.
The importance of early detection
Early detection of PKD is critical for effective management of the disease and slowing its progression. Regular check-ups, especially for individuals with a family history of PKD, can lead to early diagnosis and intervention. Early detection allows healthcare providers to implement treatment strategies to preserve kidney function and improve the patient’s quality of life.
If you suspect that you or a loved one may have PKD, seek medical advice and support from healthcare professionals who specialize in kidney diseases.

